The impact of migraine in New Zealand

Migraine disease is estimated to affect over 733,000 people in Aotearoa New Zealand
The study measures the impact of diseases on death rates and disability, including ‘years of life lived with disability’ (YLD). Migraine is not a fatal disease but it causes significant impairment, so the YLD measure provides a way to quantify the amount and severity of this impairment.
Health and disability impact of migraine
Years of life lived with disability (YLD) calculates the number of years that a person lives with impaired function. It combines an estimate of how common migraine disease is in the population with the amount of time spent with impaired function (e.g. the frequency and duration of migraine attacks) and a number called a ‘disability weight’. The disability weight is taken from large surveys where participants compare and rate the health status of individuals with differing levels of disease and disability.
In 2023, the Global Burden of Disease study found that migraine caused the sixth-highest amount of YLD worldwide. In New Zealand, migraine has a similar disability impact to major depressive disorder. The high level of disability is consistent with what we know about the impact of migraine disease on life and functioning.
The 2023 Global Burden of Disease study also estimated that the burden of migraine, measured by YLD, was a little more than double (2.1 times greater) in females compared to males, because females with migraine spend more time with headache than males.
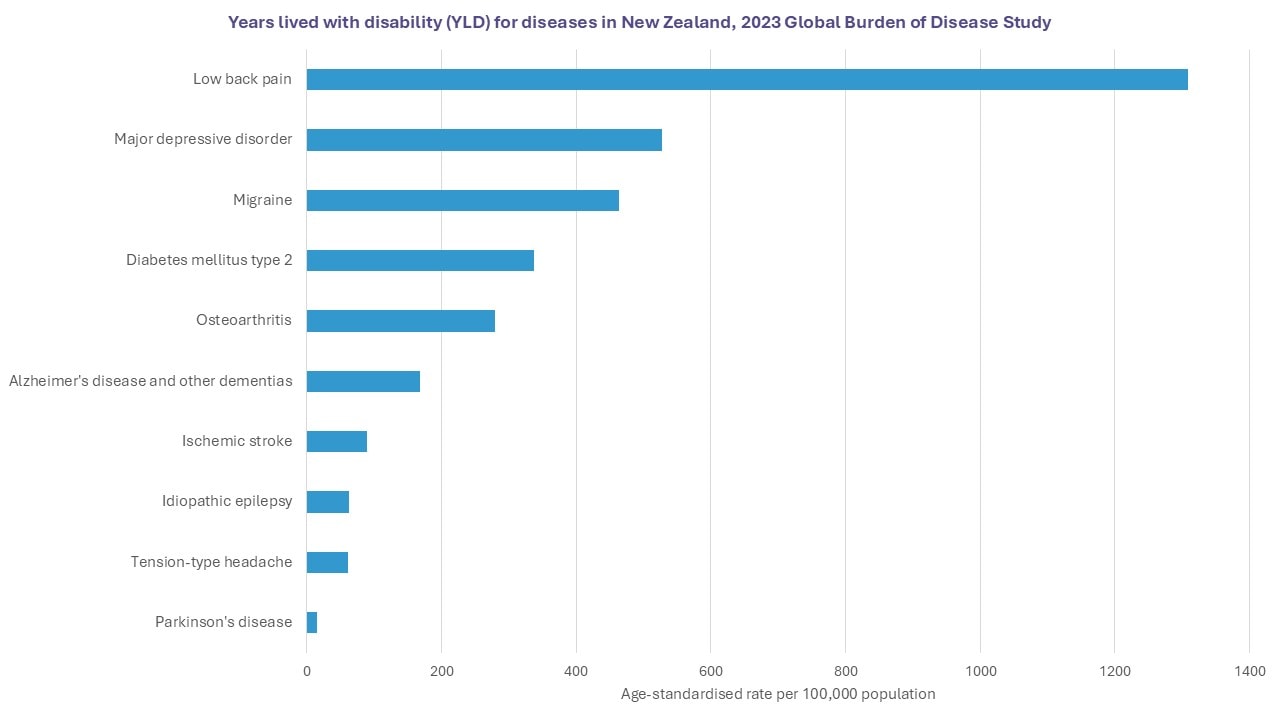
Based on Global Burden of Disease 2023 data (http://ghdx.healthdata.org/gbd-results-tool, accessed June 2024)
Social and economic cost of migraine
Migraine disease is most common in people of working age, and two to three times more common in women than men. Migraine can affect people’s ability to work, study, progress in their careers and engage in social activities and family life.
Although there is no published research on the economic costs of migraine in Aotearoa, research from Alberta, Canada (which has a similar population size to New Zealand) in 2025 predicted that health care costs were 1.5 times greater for people with migraine, corresponding to an additional annual cost per person of CAD$5,059 for people with chronic migraine and CAD$669 for those with episodic migraine.
If these estimates are similar for New Zealand, that would equate to more than NZ$1 billion a year, just for health care costs. From other research, we know that the cost from lost productivity – not being able to work during migraine attacks or work as effectively or work at all – is much greater than health care costs.
Research into the impact of migraine in New Zealand
In 2022, we undertook a nationwide online survey of people with migraine, resulting in 530 responses. This was the first research into the experience and impact of migraine in Aotearoa New Zealand.
Summary of findings
- Migraine impacted on paid and household work for the majority of respondents, especially those with chronic migraine.
- People reported difficulties in getting effective (and knowledgable) health care for migraine, especially being able to see a neurologist.
- Nearly three quarters of respondents were eligible for preventive treatment, based on frequency and disability from migraine attacks, but only 57% of these were currently taking a preventive.
- There was a clear need for new and more effective medication options, with fewer side effects.
- Just over half were using a migraine-specific acute treatment (a triptan) but risk of overuse of acute treatments was high for people with chronic migraine.
- Most people were using or had previously used supplements but other non-medication approaches were less commonly used.
- It took on average six years from having migraine symptoms to getting a diagnosis. 71% of respondents had a family history of migraine. Many felt judged or misunderstood because of migraine by family and friends, health professionals, partners and workplaces, a sign that migraine stigma is alive and present.